The latest scientific studies on psychostimulants, the medication we give to our children with ADHD, clearly demonstrate the benefits they have on their brain development in the long term. A better attention offered by the psychostimulant allows a more effective development of the executive functions of the brain in general, and promotes learning of all kinds. In addition, they greatly help with their social integration, by allowing them to be more attentive to others, and to have more appropriate behaviors. By reducing impulsivity, agitation and helping in the management of emotions, among other things. That said, the purpose of this article is not to talk about the benefits of medication, but rather to get to know it well, so that it remains helpful for parents who make this choice for their child. Because if used incorrectly or in too large a dose, we can quickly find ourselves in the hell of adjustments and side effects. However, if you want to better understand the positive impacts of psychostimulants on brain development in children with ADHD, I suggest you read the research in neuroimaging, with reference to the end of the article.
What you need to know
First, ADHD is cyclical! It’s still hard for researchers to understand why, but it seems that the brain with attention deficit disorder goes through ups and downs in its functioning. The person will have 2-3 positive weeks, where they feel good and function at their best. Then comes a period of a few days, when the brain becomes confused and struggles to function on a daily basis. The person with ADHD then becomes more anxious, more irritable and the symptoms return at a gallop. I call these moments of dysfunction, the « slump or the ADHD bug. » Like a computer that slows down and never finishes charging, the ADHD brain loses its efficiency and connections are limited.
This moment lasts from a few days to a week or so. And as if by magic, once the brain is « debugged », it returns to its normal functioning. At least, as he can be at his best. This is why your child goes from being an affectionate little kitten, relatively functional despite his ADHD, to completely lost, forgetting everything, becoming anxious, irritable, even oppositional and very unpleasant. The teacher then writes you a note in the diary, asking if you have given her her medication, describing difficult behaviors during the day. And yet, you give it every morning without exception. It is normal, for both children and adults, to have effective periods and slow periods. The ADHD brain has a « little bug » from time to time! Once he puts everything back in the right boxes, he will return to his normal functioning as we know it, at its best.
Once we understand this, it’s important to understand that medication doesn’t take away this cycle at all! It will always remain. However, during the effective period, your child will be even more functional with the medication. And during the off-peak period, it will be less important than without medication.
To recognize cyclical episodes, I always suggest that parents for at least two consecutive months write on the calendar whether the day was generally good, average or difficult. Maybe with a green, yellow, and red color code. This way you will see how long the cycles last, and you will better identify when the slow periods arrive. During these times, we reduce activities and it may not be the right time to ask too much of your child. Conversely, during its good periods, we can take advantage of it.
This increases the intensity of off-peak periods
Fatigue
Lack of sleep
Stress
A more demanding time in life (moving, exam period, etc.)
Family tensions
Poor diet
Lack of physical activity
The disease
For adults, consumption in general
Start taking medication
Medication has its own chemistry and the body has its own chemistry. Integrating a new molecule into the system, the body has to get used to it. It is therefore normal that this changes the functioning of your child’s internal system for a while. Once the body gets used to it, it should normally have no more adverse effects. We must give the body time to learn to manage and tolerate this new molecule. It is therefore important to follow the integration sequence proposed by the doctor. As parents and caregivers, let’s take advantage of this integration time to observe the positive and negative effects that we notice. Write them down to share with the pediatrician later. Also ask his teacher what he observes. If your child is old enough, ask them to observe how their days go. It is also important to take the time to see if the negative effects fade. They can last a few days, but disappear completely if you give yourself the necessary time, and the molecule is really appropriate for him. As presented in the table of the Canadian ADHD Practice Guideline, which is a visual below, the first dose to start is minimal. The doctor may suggest that you adjust it if necessary, depending on your child’s weight and age. With the doctor’s agreement, supported by the pharmacist, it can be increased later, if you judge together that it has little effect. If the effects are positive, no matter the dose, and we have the impression that our child is at his best, WE DON’T TOUCH IT ANYMORE.
One important mistake we make regularly is not considering the ADD(H) cycle. There will always be slow periods. The teacher calls us to say that things haven’t been going well for a few days at school, and you, too, have noticed that it’s a more difficult time at home. So everyone says to themselves that « we need to increase the medication ». No, not at all! It’s probably just a slow period. Medication or not, it will appear eventually. The total cycle lasts about a month: total of good and not so good periods. A bit like the menstrual cycle. 😉 Wait at least a week to see if the slow period finally passes, before even calling the doctor for a raise. If it passes and everything goes back to normal, WE DON’T TOUCH THE MEDICATION.
If we increase it during the off-peak period, your child may find himself overdosing when it passes. Then you will fall into the adverse effects of too much medication. Too much medication is worse than not giving it. In too large a dose, psychostimulants make the child even more agitated and hyperactive. They bring a form of excitement and internal anxiety. They increase irritability, suppress appetite further and interfere with sleep. Your child will seem even more ADD(H)! He may even become more aggressive and oppositional. But it’s not necessarily the medication that’s not appropriate for your child, but rather that they’re overdosing. If the previous dose gave good results, we do not change the medication. We only return to the previous dose. If everything goes back to normal, WE DON’T TOUCH IT ANYMORE.
Medication does not make ADHD disappear
The next and most important mistake is to think that medication makes ADHD disappear. Attention deficit disorder is a neurobiological difference in the brain itself, and it will remain no matter what medication is given. Medication reduces symptoms and helps your child be more attentive. Attention being the gateway to his brain, if it is very weak, it will develop less well. If it is increased by medication, the brain will be able to make more connections in the short and long term, and possibly function better. But since we want to have perfect results as if by magic, we bet everything on medication in the « here and now ». This is true for parents, but also for school workers who would like medication to solve all problems. Medication has its limits. Once the right dose has been taken, the remaining difficulties must be overcome by ADD(H) adaptations.

The last mistake that often comes up is to think that all of a sudden, the medication that has been working so well for months or years, no longer works. With few exceptions, if it worked well, there is no reason for it to become problematic overnight. Very often, problems occur when we have increased the medication. Having had a difficult period, we tell ourselves that the medication « no longer works ». We then increase and we find ourselves in the unhealthy cycle of overdose. The side effects of an overdose are similar to the symptoms of ADHD. Then we think that the drug no longer works. NOT TOO FAST! Before anything else, go back to the previous dose to see if everything returns to normal. If this is the case, WE DON’T TOUCH IT ANYMORE.
Increasing medication because it no longer has enough effect should happen very rarely and for very logical reasons. For example, that your child has gained several centimetres in the last year and that not a single pair of pants fits him anymore. But still! Your child’s weight must have increased significantly to actually require a significant increase.
Effects
Again, being a form of « body chemistry, » your child may respond less well to one kind of medication and better to another. What is important is to find the right molecule for your child. The best sign that medication is right is that your child is working at their best, based on what you know about them. It will not change with medication. He will remain himself. But medication should lead him to be at his best, if it is well adjusted. That said, there will still be TDA(H) bugs. This is normal. We have to consider them. But with good medication, off-peak periods should be less intense. The side effects should almost completely disappear, giving the body time to adjust.
The side effect, which normally remains regardless of the medication, is a decrease in appetite at lunchtime. The medication gives its full effect at the end of the morning and therefore, it is at this time that the appetite is reduced. But it’s okay at all if your child eats well in the morning and evening. That he makes up for it with healthy snacks during the day. The other effect often observed is difficulty falling asleep. Often, it’s because we give the medication too late in the morning. Long-lasting medications take effect for 10 to 12 hours. Although the beneficial effects have ceased, the drug can still make it difficult to sleep two hours after it disappears from the system. So, especially for the little ones who have difficulty falling asleep and who react more to medication, we need to count on 12 to 14 hours of effects. So if you give the medication at 8 a.m. and he goes to bed at 7 p.m., the chances that he will have difficulty falling asleep are significant.
To solve the problem, it must be the first thing we give him in the morning. The medication takes about 30 minutes to take effect. He will have time to eat before the potential loss of appetite. The morning routine will also be more enjoyable, as you too will benefit from better attention in your child.
Families of psychostimulants
Here is the table of ADD(H) medications from the CADDRA guide, which we can easily find on the web. It shows you the families of drugs used for pharmacological treatment. The best known are methylphenidates, the Ritalin family, Biphentin, Concerta and Foquest. They are normally the ones we start with, as they are the most studied and well-known in the treatment of ADHD. They also often give fewer side effects. If we refer to this reference guide, Ritalin lasts about 4 hours and should be given to children in the morning and at noon, which makes it less interesting. We then have to ask school workers to give the second dose, which complicates things. The Biphentin and the Concerta are long-lasting. Therefore, only one dose per day is normally required. Concerta is the most controlled and stable in its release, given its pusher compartment, which quietly releases the dose throughout the day.
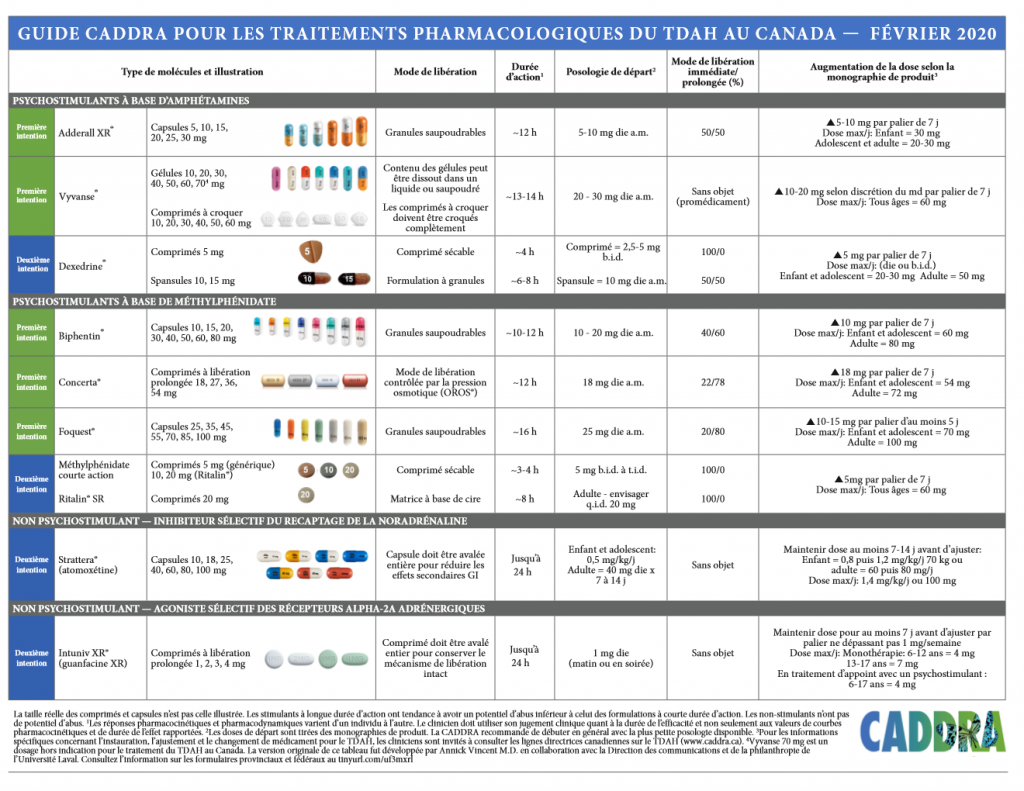
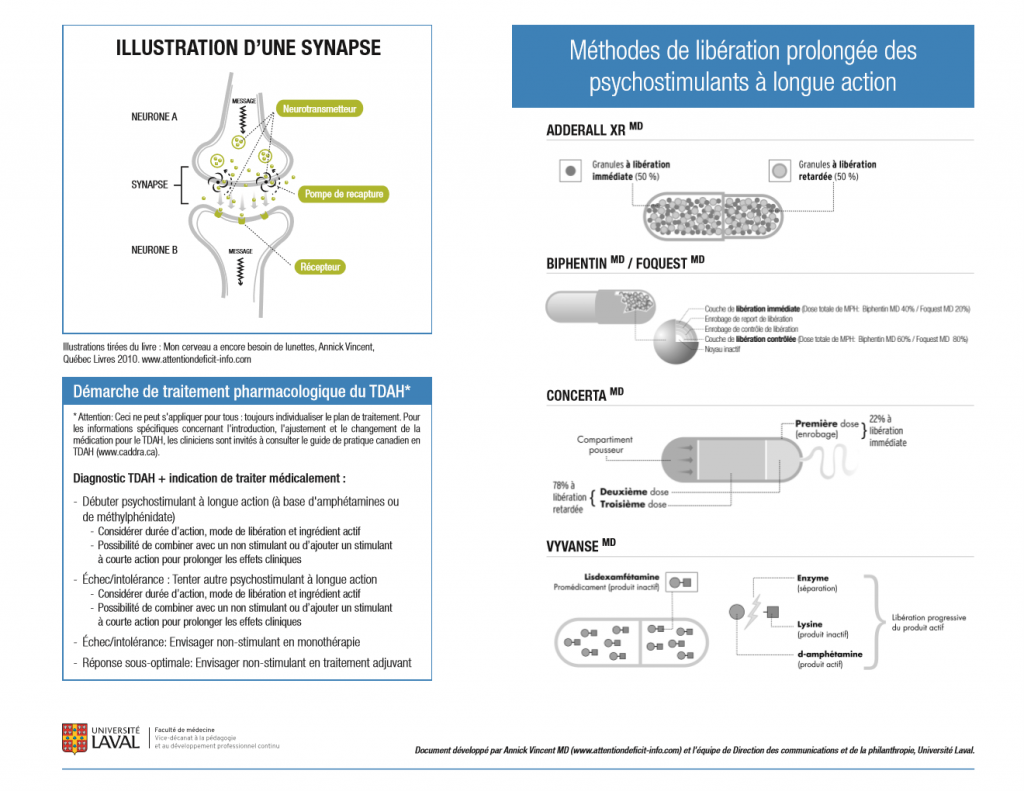
The second family is amphetamines, such as Vyvanse and Adderall. If the child reacts less well to the Ritalin family, the pediatrician often tries the second one to check if the effects are better. Note, however, that a child may react very differently to two medications in the same family. For example, my two boys reacted badly to Biphentin (lots of side effects), but my oldest reacted very well to Concerta from the same family. My youngest, not swallowing the pill, we turned to Adderall, which does a very good job at home. Some drugs are tested because the child cannot swallow the pills. Biphentin and Adderall, for example, open and can be taken with compote or yogurt for example.
There are two other drugs that are not part of the psychostimulants, such as Strattera and Intuniv, which are normally tested when the first two families give worse results. Often to accompany a psychostimulant, by treating different ADD(H) effects. For example, an attention pill, and another that targets impulsivity more specifically.
It is important to develop a team partnership with your child’s doctor. It will always be the doctor and the pharmacist who will remain the specialists in medication. Our role as parents and caregivers is to provide as much concrete and relevant information as possible at the appointments, so that the doctor can make the best decision. Hence the importance of writing down your observations in a notebook, for example, during the trial period. Be objective. There is a noticeable difference in the quality of information according to the following sentences: « my child has sleep disorders » and « once or twice a week, he has trouble falling asleep. » Or again, « that he no longer eats, » as he is, « at school he has little appetite, but he eats well at supper and takes several snacks. » The more accurate the information, the more they will be able to help you. And don’t forget about the slow periods. There will be better times and not so good times.
When the medication « arrives »
The medication has supported your child’s brain all day, but at suppertime, she hangs up her apron. She’s done her job, finished her day, and she’s leaving your child’s body. The brain then finds itself pedaling on its own. The ADHD in all its glory is back at the helm. It is normal to observe a period of increased agitation or a form of disorganization that lasts about 30-45 minutes when the medication no longer works. The brain must regain control of its usual ADD(H) functioning without the medication. There is a normal adjustment that is observed and that often leads to an increase in behaviour. And of course, it’s often around supper time that it happens.
Your child was quiet five minutes ago, and suddenly he becomes a tornado. We must therefore plan these moments to better manage them and keep our patience. After the short period of readjustment, normally the small tornado passes and the child returns to normal, in what he is without the medication. Again, this « after medication » period is unrelated to the medication itself. If your end of the day is difficult, talk to your doctor. But the solutions will be found more in the adaptations that you will have to put in place to have better evenings.
You will find many tips and tricks in many of my articles on ADHD on the Hapax blog and on the Facebook page. To better accompany our little ones who are sometimes restless or in the moon, that we love so much! We hope that this article guides you on your journey in medication. It’s better to take it slowly, but to make good progress to get good results. And for parents, remind teachers that the adjustment will take some time, and that ADHD does not go away. Adaptations will always have to be on the menu to help these children, even if they are well medicated. Why not share this article with them, so that you can all start on the same foot, and be a great close-knit team to support your child.
RESEARCH ARTICLES
Psychostimulants would have a positive effect on the brain development of young people with ADHD, by the CERC (Nov.2015).
Spencer TJ, Brown A, Seidman LJ, et al. Effect of psychostimulants on brain structure and function in ADHD: a qualitative review of the literature of neuroimaging studies based on magnetic resonance imaging. J Clin Psychiatry . 2013; 74(9):902-917. doi:10.4088/JCP.12r08287
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3801446
Ivanov I, Murrough JW, Bansal R, Hao X, Peterson BS. Cerebellar morphology and effects of stimulant drugs in youth with attention deficit hyperactivity disorder. Neuropsychopharmacology . 2014; 39(3):718-726. doi:10.1038/npp.2013.257




Leave a Reply